Our solutions +
You drive what we do. Our flexible, bilingual, white-label business solutions are branded and customized to your specifications. We offer advanced technology, innovative claims management, and administrative services – you choose the combination of products and services that will address your business needs.
One system is all you need
HBM+ business solutions are first and foremost built on technology. And all of our technology is based on the Advantage system. It is a single streamlined system that handles all health benefit categories for claims management and all aspects of plan administration, including:
- Processing plan member enrolment and information, and benefit plan changes
- Plan member eligibility
- Accurate, real-time adjudication for all types of claims
- Health care provider management, overseeing professional guidelines, fraud and abuse, and regular and customary pricing
- Claim payments and statements
- Reporting that can be customized to meet client needs
- Online services for plan members, administrators and health care providers
Powered by Advantage
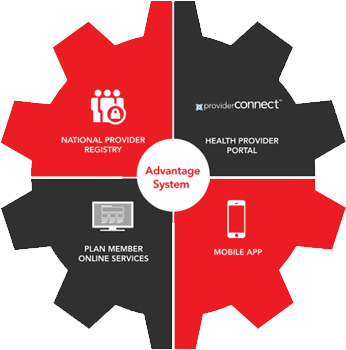
Powered by Advantage
HBM+’s automated, flexible, patient-centric, and rules-based health benefits management system completely integrates claims adjudication with administration. This is what we mean:
- Data (like plan changes, pricing, or provider details) is available in real-time
- Fully scalable system architecture provides capacity on demand at no additional cost
- A comprehensive library with thousands of rules can accommodate any plan design
- Coordination/integration of benefits with provincial drug programs
- Electronic administration of coordination of benefits claims
- Plan members can automatically coordinate unreimbursed claim amounts with health care spending accounts
Customizable based on your needs
Our flexible, white-label business solutions are branded and customized to your specific needs. You choose the combination of products and services that will fit your business needs. Here are just two solutions we provided to clients that had very different requirements.